Pediatric behavioral health: When to screen and how to bill
Approximately 1 in 5 children in the United States suffers from a diagnosable mental disorder but only 20% to 25% of affected children receive treatment1.
Mental health disorders and behavioral health issues in children and adolescents
According to the American Psychological Association (APA) half of all mental health issues start by age 14 and three-fourths before age 242 . According to the Substance Abuse and Mental Health Services Administration (SAMHSA), more than 40% of youth ages 13 to 17 have experienced a behavioral health issue by the time they reach seventh grade, and upwards of 90% of substance use disorders begin during the teen years. Additionally, they report that suicide is the third leading cause of death (after accidents and homicide) among youth ages 15 to 243.
The impacts of mental health disorders
The CDC published a report in 2013 that indicated people with mental disorders frequently have more than one type of disorder, with an estimated 40% of children with one mental disorder having at least one other mental disorder. The report also indicated that children with mental health disorders more often have other chronic health conditions (e.g., asthma, diabetes, and epilepsy) than children without mental health disorders4.
Compared with their peers, children and adolescents with mental health needs are more likely to have housing instability, have interactions with the justice system, be delinquent from school or not finish school, and be underemployed5.
SAMHSA-HRSA Data about Co-Occurring Chronic Health Conditions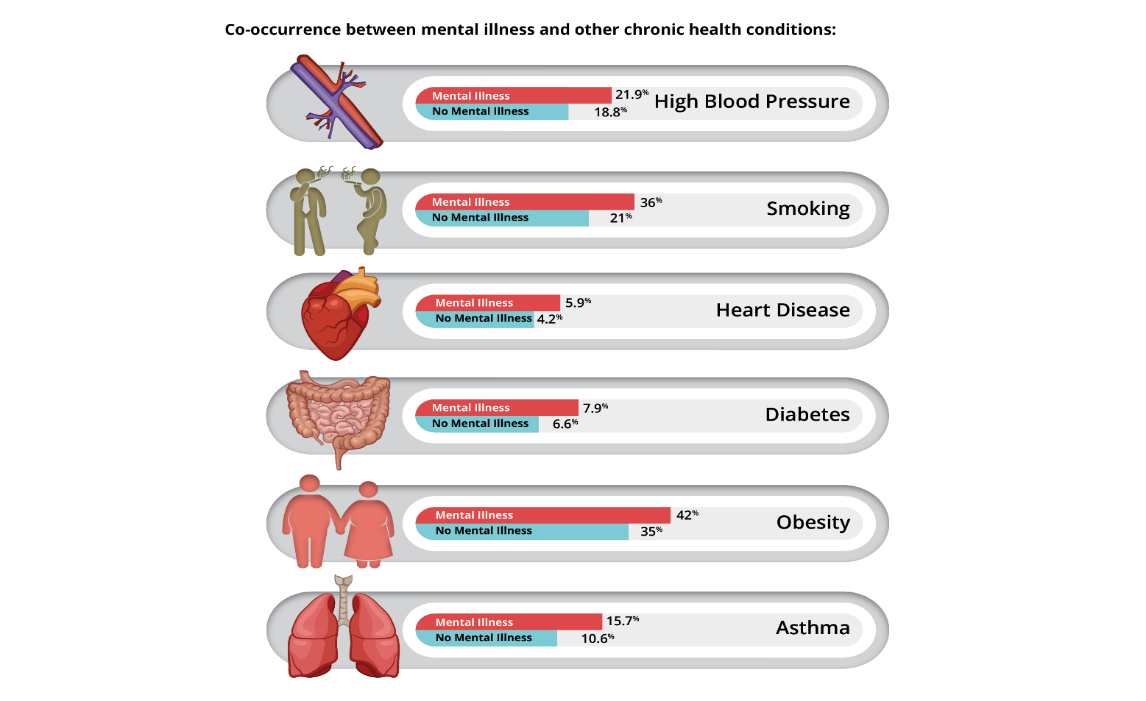
The importance of behavioral health screening
Given the significant effects of mental health (MH) and substance use (SU) disorders as well as the increased risk for comorbid medical conditions in youth with MH and SU disorders, it is critical that children and adolescents be screened and referred for appropriate care when mental health symptoms and substance use habits are identified. The National Institute of Mental Health indicates that, for a young person with symptoms of a mental health disorder, the earlier treatment is started, the more effective it can be6. Early treatment can help prevent more severe, lasting problems as a child grows up. According to the CDC, primary care providers are seeing more children and adolescents than any other medical provider7. As such, it is essential to integrate regular mental health screenings into primary care visits.
State Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) guidelines require that states provide regular health screenings and all medically necessary services to children and adolescents, including assessments of mental health. MassHealth requires that primary care practitioners offer to screen children and youth, birth through age 20 (or their families), for potential behavioral health (BH) conditions during office visits, using approved standardized BH screening tools. All primary care providers caring for MassHealth children under the age of 21 must offer 1 of 8 standardized BH screens at each Well Child visit.
Coverage and billing for preventive developmental screening
While primary care providers seeing privately insured children and adolescents do not have the same requirements to offer behavioral health screening to their patients, it is vital to screen all children and adolescents using appropriate tools. MH and SU disorders impact youth across all demographics. To encourage screening for all children and adolescents, preventive developmental screening is covered and reimbursed when performed as a component of the preventive well visit.
Providers can bill for one screening per member per day with an add-on service code of 96110 and one of the U-modifiers listed below.
|
Behavioral Health Screening Tools |
Administrator |
Age |
|
|
ASQ:SE |
Parent |
6 to 60 months |
|
|
BITSEA |
Parent |
12 to 36 months |
|
|
CRAFFT |
Car, Relax, Alone, Forget, Friends, Trouble (specific to substance/alcohol use) |
Youth |
14 to 21 years |
|
ECSA |
Parent |
18 to 60 months |
|
|
EPDS |
Edinburgh Postnatal Depression Scale (new as of March, 2017)
|
Parent |
0 to 6 months |
|
M-CHAT |
Modified Checklist for Autism in Toddlers (specific to autism (for dates of service through 12/31/17 only—effective 1/1/18, only the MCHAT-R can be use) |
Parent |
16 to 30 months |
|
M-CHAT-R/F |
Modified Checklist for Autism in Toddlers (revised with follow-up) |
Parent |
16 to 30 months |
|
PEDS |
Parent |
Birth to 8 years |
|
|
PHQ-9 |
Youth |
13+ years |
|
|
PSC/PSC-17 |
Pediatric Symptom Checklist or 17-question version (new as of March, 2017) |
Parent |
4 to 16 years |
|
PSC-Y |
Youth |
11 to 18 years |
|
|
PSC-17 |
|||
|
SDQ |
Parent |
3 to 16 years |
|
|
SDQ |
Youth |
11 to 16 years |
|
|
SWYC or SWYC-MA |
Survey of Wellbeing of Young Children (standard or Massachusetts specific version) |
Parent |
0 to 60 months |
U-modifiers for billing
|
Modifier |
Standardized behavioral health screening is |
Was a BH |
|
U1 |
physician, independent nurse midwife or independent nurse practitioner |
No |
|
U2 |
physician, independent nurse midwife or independent nurse practitioner |
Yes |
|
U3 |
nurse midwife employed by a physician |
No |
|
U4 |
nurse midwife employed by a physician |
Yes |
|
U5 |
nurse practitioner employed by a physician |
No |
|
U6 |
nurse practitioner employed by a physician |
Yes |
|
U7 |
physician assistant employed by a physician |
No |
|
U8 |
physician assistant employed by a physician |
Yes |
Resources
If a member screens positive for behavioral health issues, is not currently engaged in treatment, and is agreeable to treatment, here’s what you can do.
Optum resources
Optum is our behavioral health partner, and they have resources available to help you care for members with behavioral health concerns
- Search for a provider on Optum’s Live and Work Well Website
- Call and request a list of providers for behavioral health services
- Optum Customer Service:
844-451-3519
Hours: Weekdays 8:00 AM to 6:00 PM except Thursdays when they are available from 8:00 AM to 8:00 PM
- Behavioral health clinicians are available for urgent issues (e.g., prior authorization requests) 24-hours per day.
Other resources for all members
- Check the list of behavioral health services and providers on the AllWays Health Partners’ website
- If a member is in crisis and in need of an emergency evaluation, emergency service providers (ESPs) are available 24 hours a day, 7 days a week, 365 days per year via the Statewide ESP hotline, 877- 382-1609. Call this number and enter your zip code to get the toll-free number for your local ESP. You can find more information on the State's ESP page.
- Massachusetts Child Psychiatry Access Program (MCPAP) provides free consultations on how to integrate behavioral health in primary care settings.
Resources for My Care Family members
- Work with Merrimack Valley Accountable Care Organization (MVACO) Care Teams to request assistance in making a referral for behavioral health services
- Explore services available on the MABHA website, which includes an overview and resource materials on youth and family services as well as MH and SU services
Resources for Commercial and Partners ASO members
Refer members for care coordination or care management services through AllWays Health Partners by calling the phone number on the back of the member’s ID card.
____________________________________________________________________________________
[1] A. (2009). Improving Mental Health Services in Primary Care: Reducing Administrative and Financial Barriers to Access and Collaboration. ACADEMY OF CHILD AND ADOLESCENT PSYCHIATRY Pediatrics,123(1248). doi:10.1542/peds.2009-0048
[2] Ward-Zimmerman,PH.D, B. (2012). The Integration of Routine Behavioral Health Screening Into Pediatric Primary Care. APA Annual Convention.
[3] Ann.lynsen. (2014, September 24). Age- and Gender-Based Populations. Retrieved from https://www.samhsa.gov/specific-populations/age-gender-based
[4] Mental Health Surveillance Among Children - United States, 2005–2011. (2013, May 17). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/su6202a1.htm
[5] Mental Health Surveillance Among Children - United States, 2005–2011. (2013, May 17). Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/su6202a1.htm
[6] Child and Adolescent Mental Health. (n.d.). Retrieved from https://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health/index.shtml
[7] National Ambulatory Medical Care Survey: 2015 State and National Summary Tables. (2015). U.S. Department of Health and Human Services- Centers for Disease Control and Prevention National- Center for Health Statistics.