Black women face a barrier of racial & gender bias in healthcare
As part of Women's Health Month, we're focusing on the inequities women of color face within our healthcare system. People of color face inequalities across the board, and the pandemic has only magnified this grim reality. Black men and women are at much higher risk of contracting COVID-19 than the rest of the population, and they are 2.1 times more likely than white people to die from the virus. That's why Black women are left to face a double edge sword of discrimination due to race and sex, and research shows especially how dangerous this reality is in healthcare.
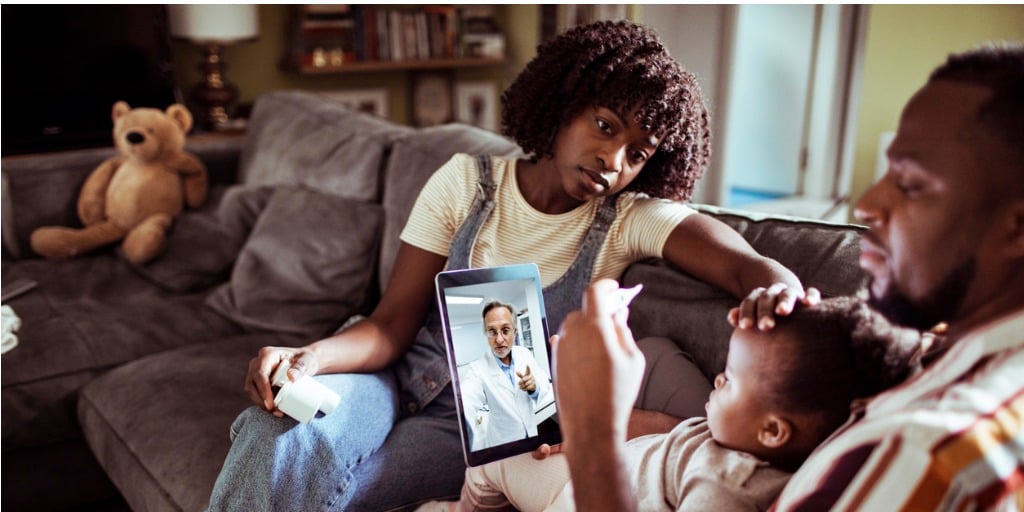
Fighting for healthcare
Just ask Elizabeth Galvin. After a severe car accident, she suffered from severe back pain on and off for years. Guess what her doctors said. They told her that her back pain was due to her weight. Her pain continued, and her doctor recommended weight loss surgery and told her to focus on nutrition. Two years later, another doctor discovered Galvin had a severe misalignment of her spine—as you might have guessed—from the car accident. She got the physical therapy she knew she needed all along but still felt disempowered. She told TODAY, "I asked for pain meds but was careful because I didn't want seeking behavior noted in my chart."
Discrimination in the U.S. healthcare system leads to healthcare inequities that fuel oppression. A 2017 study in the journal Critical Public Health noted that health care inequities exist for Black women across socioeconomic statuses. The research notes that Black women have to work that much harder to fight against normalized stereotypes during interactions with their doctors. This aligns with one study that found that white adults without medical training endorse beliefs about biological differences between Black and white individuals, many of which are false. Here are just some of the assumptions participants were asked to form an opinion on:
- Black people age more slowly than white people
- Black couples are significantly more fertile than white couples
- Black people have denser, stronger bones compared to white people
- White people have larger brains than Black people
- White people are less susceptible to heart disease than Black people
- White people have a better sense of hearing compared to Black people
- Black skin is thicker than white skin
- White people have more efficient respiratory system than Black people
- Black people have a stronger immune system than white people
This same study took it one step further by surveying white adults with medical training. These individuals were asked the same questions mentioned above. Additionally, they were asked to give a pain rating and a treatment recommendation on two mock medical cases—one for a white adult and one for a Black adult. On average, participants endorsed 11.55 percent of false beliefs of comparisons between Black and white people. About 50% reported that at least one of the false belief items was possibly, probably, or definitely true. They also found that participants who endorsed more false beliefs rated the Black target as feeling less pain than the white target.
Alarming death rates linked to Black women
According to the CDC, "Black, American Indian, and Alaska Native (AI/AN) women are two to three times more likely to die from pregnancy-related causes than white women – and this disparity increases with age." This statistic is especially startling as the CDC also claims that about 3 in 5 pregnancy-related deaths could be prevented. Another report found that delays in follow-up care result in higher mortality rates after a breast cancer diagnosis.
So why are Black women at a higher risk for pregnancy complications? According to the University of Chicago Medicine, the answer is systemic racism. Racism blocks Black women from access to quality healthcare which puts them at a higher risk of pregnancy complications. In the U.S., maternal complications and death are caused by heart disease, infection, embolism, and hemorrhage. Although these are all treatable, they become life-or-death illnesses when bias blocks Black women from quality healthcare resources—and even testing.
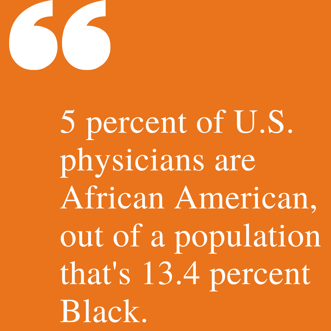
A 2016 Journal of Clinical Oncology study found that black women, regardless of their risk level, are less likely than white women to undergo genetic testing—in large part because physicians are less likely to recommend it to them. This is a result of the lack of diversity within the healthcare system. According to the Association of American Medical Colleges, of all active physicians—only 5 percent are Black—and only 2 percent are Black women. For added perspective, 13.4 percent of the U.S. population is Black.
Nancy Krieger, Ph.D., a social epidemiology professor at Harvard T.H. Chan School of Public Health, has found a link between Jim Crow laws and premature mortality rates for African-Americans born under those laws. Krieger cites potential reasons for the link, including lack of access to adequate medical care, excess exposure to environmental hazards, economic deprivation, and the psychological toll of dealing with racism as a part of daily life. Aligned with Krieger's research, The Article That Could Help Save Black Women's Lives added noted that Black women born before 1965 in Jim Crow states are to this day more likely than those born at the same time in other states to have estrogen-receptor negative breast tumors, which are more aggressive and less responsive to traditional chemotherapy.
What can healthcare professionals do?
As a healthcare professional, you can take several proactive steps to change these dire statistics. You can reevaluate biases you may be making without cognizance. You can speak out where you see racism in the workplace. You can listen to Black patients and moms. You can ensure your offering Black women the full spectrum of care and throwing away all stereotypes. If you're unsure where to start, learn more about SPEAK UP Champions and their mission to expand the use of quality improvement to eliminate preventable perinatal morbidity and mortality and ensure equity in perinatal outcomes.
What the White House is doing to address the maternal health crisis
President Biden and Vice President Harris announced initial actions to improve Black maternal health including:
- Increased investment in reducing maternal mortality and morbidity
- Approval of the First Medicaid Section 1115 Waiver to Broadly Extend Postpartum Coverage
- $12 Million in Additional Funds for Maternal Obstetrics Care in Rural Communities
Read the complete fact sheet here. To learn more about how you can SPEAK UP in your community or organization, visit perinatalqi.org/page/speakup or visit the Disparities Solution Center.